|
|

The CSPCA Charitable Trust needs your support through donations to continue vital research projects. Your donation is tax deductible.

RASP (Rescue A Shar-Pei) is a volunteer group with a concern for abandoned and abused Shar-Pei in Illinois / Indiana / Wisconsin and surrounding areas.
|
 
|

|
|
Frequently Asked Questions
  
| 
Patellar Luxation
- Medial Luxations
Often these are termed “congenital” due to the fact they occur early in life and are not associated with trauma. Luxation may not be present at birth but the anatomical deformities that predispose to these luxations are present at that time and are responsible for later problems.
The occurrence of medial patellar luxation is characterized by:
- Coxa vera — which is a decreased angle of inclination of the femoral neck.
- Genu varum — in which the distal third of the femur is bowed medially.
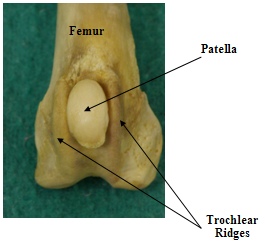
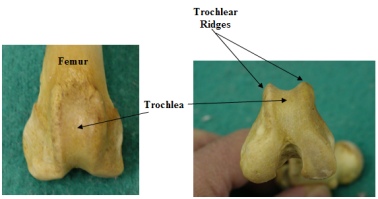
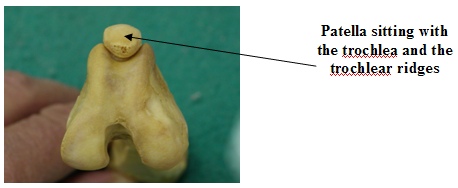
- A shallow trochlear sulcus with poorly developed or absent medial ridge.
- A hypoplastic medial humeral condyle resulting in tilted stifle joint.
- A decreases in femoral neck anteversion.
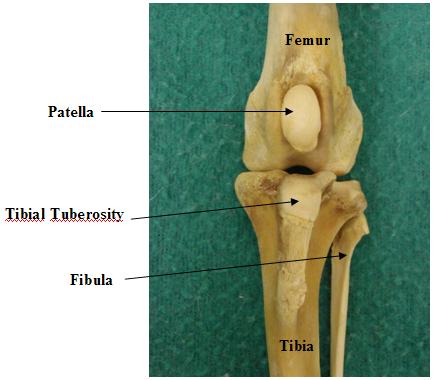
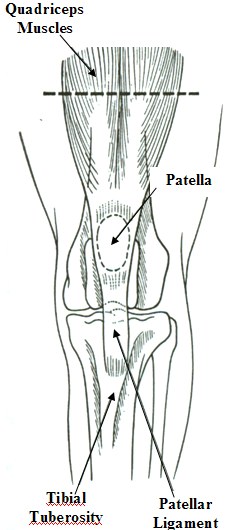
Medial luxation is much more common than lateral luxation in all breeds representing 70-80% of the cases with bilateral involvement seen 20-25% of the time. Chronic luxating patellas seem to predispose to anterior cruciate ligament rupture due to the forces exerted on the ligament by the abnormal alignment of the quadriceps mechanism. The quadriceps mechanism consists of the quadriceps muscle groups on the front of the thigh, the patella, the trochlear groove, the straight patellar ligament and the tibial tuberosity (The attachment of the patellar ligament on the upper aspect of the lower leg). Patellar luxation is graded based on the following scale:
Grade I — - Intermittent patellar luxation causing the limb to be carried occasionally.
The patella luxates at full extension but returns to normal position when
released. With the patella in normal position the leg aligns normally.
Grade II — - Luxation occurs more frequently than in Grade I. The patella luxates
easily. There is slight external rotation of the leg. Many dogs live with this
grade for years before progressive arthritis causes more severe lameness.
Grade III — - Here the patella is permanently luxated with very noticeable external
rotation of the leg. The trochlea shallow or flattened. There is moderate
lameness.
Grade IV — - The patella is permanently luxated and the limb may be carried if
unilateral. If bilateral the dog may move in a crouched position in the rear
end with the limbs partly flexed and severely “toed-out”.
- Lateral Luxations
Lateral patellar luxation is also known as genu valgum. Components of hip dysplasia such as coxa valga (increased angle of inclination of the femoral neck) and increased anteversion (excessive external rotation of the upper part of the femur relative to the lower part) of the femoral neck are seen in this condition. These deformities result in internal rotation of the femur which displaces the quadriceps mechanism and patella laterally (externally). The most common finding is a knock-knee (genu valgum) stance.
In mild cases surgical repair may not be necessary. Signs may worsen as the dog gains weight, joint cartilage erosion occurs, the luxation becomes permanent, the cruciate ligament ruptures or hip problems develop. Surgical repair can consist of soft tissue reconstruction or
bone reconstruction or both.
Without going into the actual surgical techniques I will list the soft tissue reconstruction procedures available:
- Overlap of the lateral or medial retinaculum
- Fascia lata overlap
- Patellar/Tibial antirotational suture ligaments
- Desmotomy/Capsulectomy
- Quadriceps release
The bone reconstructive procedures consist of:
- Trochleoplasty
- Trochlear chondroplasty
- Recession sulcoplasty
- Trochlear sulcoplasty
- Transposition of the tibial tuberosity
- Patellectomy
- Osteotomy
Post-operative care involves limiting exercise for 3-4 weeks with particular attention to preventing jumping. Post-op pain medication may be dispensed as indicated. Later, physical rehabilitation will be needed.
|
|
|

